Abstract
Background: Due to new imaging modalities such as low-dose whole body CT, MRI, and PET-CT which are characterized with high sensitivity and specificity extramedullary disease (EMD) is identified more frequently in patients (pts) with multiple myeloma (MM). There is not enough data concerning comparison bone marrow (BM) and EMD tumor morphology features.
Aims: Comparison of BM biopsy histopathological examination results of MM pts with osseous plasmacytomas, extraosseous plasmacytomas and MM pts without EMD. Comparative analysis of osseous and extraosseous plasmacytomas biopsy features.
Patients and Methods: From October 2013 to April 2017 35 pts with newly diagnosed MM (19 males, 16 females) 24-73 years old (median 56) were included in our study. The disease was diagnosed in accordance to IMWG criteria (2014). We defined EMD as osseous (plasma cell tumor extending from the intramedullary spaces of the bone marrow through the cortical bone) or extraosseous (spread to organs distant from bone) plasmacytomas. Through our pts 21 had EMD, including 14 pts with osseous plasmacytomas and 7 pts with extraosseous plasmacytomas. In 14 pts EMD was not found. In all cases BM trephine biopsy and EMD biopsy were performed. Cross-tabulation analysis was performed using freq procedure in SAS 9.4.
Results: Three histopathological variants of BM in MM pts were identified:
1. Interstitial loose infiltration with mature plasma cells, scattered among the elements of myelopoiesis, without cell aggregations.
2. Massive infiltration with mature plasma cells or their numerous aggregations.
3. Massive infiltration with immature myeloma cells (with different ratio of proplasmacyte-like and plasmablast-like cells).
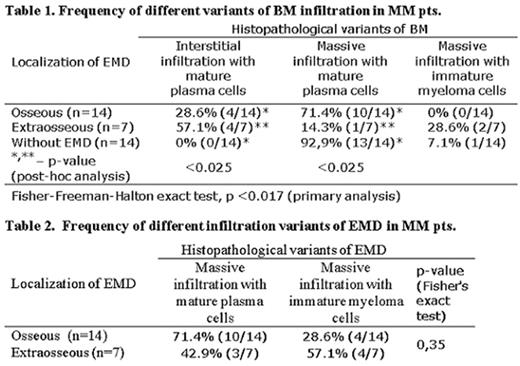
We conducted comparison of histopathologic pattern of bone marrow in MM pts with osseous plasmacytomas, extraosseous plasmacytomas and without EMD (Table 1). The groups of pts were comparable by sex, age and other clinical significant characteristics.
The tumor substrate of BM in MM pts with extraosseous plasmacytomas represented by loose interstitial infiltration with mature plasma cells was significantly more frequent (p<0.025), than in MM pts with osseous plasmacytomas or without EMD, and in those 2 groups massive infiltration of BM with mature plasma cells was prevalent.
Histopathological features of EMD were also studied (Table 2). Two histopathological variants of EMD were identified:
1. Massive infiltration with mature plasma cells;
2. Massive infiltration with immature myeloma cells (with different ratio of proplasmacyte-like and plasmablast-like cells).
The substrate of extraosseous plasmacytomas was represented by immature tumour cells somewhat more frequently in comparison with the substrate of osseous plasmacytomas (57,1% vs 28,6%), through the difference was not significant.
Conclusion: In this prospective study we found a significant difference of histopathological pattern of bone marrow in MM pts with extraosseous plasmacytomas. In contrast with the group of pts with osseous plasmacytomas or without EMD, bone marrow in MM pts with extraosseous plasmacytomas was characterised by loose interstitially infiltration with mature plasma cells. In the two other groups massive infiltration of bone marrow with mature plasma cells was seen. No significant differences were found between the morphology features of osseous and extraosseous plasmacytomas. We think that our results can be helpful in differential diagnosis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal